2018 Health FSA Limit Projection, New SF HCSO Amounts, and Revised Contraception Rules
By Brian Gilmore | Published October 10, 2017
A lot is happening this Fall, even if the anticipation of an ACA repeal/replace bill never came to fruition.
2018 Health FSA Salary Reduction Limit Likely to Increase to $2,650
The ACA limitation on health FSA salary reduction contributions was a common target for the multiple ACA repeal/replace bills considered over the course of the year. Its repeal was included in the American Health Care Act bill that passed the House, and the Better Care Reconciliation Act bill that was initially proposed in the Senate (but subsequently failed). Interestingly, the Senate’s Graham-Cassidy bill, which received a late push for passage near the end of the September 30 deadline, did not include repeal of the health FSA limit.
In any case, with no ACA repeal/replace legislation currently having any imminent chance of enactment, the limitation will remain for at least the 2018 plan year.
Newfront is projecting that for plan years beginning on or after January 1, 2018, the health FSA salary reduction contribution limit will increase to $2,650 (up from $2,600 currently). Our projection shows an inflation increase of $167.25 (from the initial $2,500 limit in 2013). By law, the increase is rounded to the next lowest multiple of $50, which in this case will be an increase of $150 from the initial $2,500 limit.
The increase will not be official until the IRS releases its annual inflation-adjusted limits. The IRS issues those numbers in a Revenue Procedure document that typically comes out in late October. Last year, the release date was October 25. Stay tuned.
As a reminder, employer contributions (including non-cashable flex credits) cannot exceed $500 per plan year for the health FSA to maintain excepted benefit status. Non-excepted health FSAs generally cannot comply with the ACA market reform mandates. Therefore, in almost all cases, the maximum health FSA amount available to an employee for plan years beginning on or after January 1, 2018 will be limited to $2,650 (max employee salary contribution) + $500 (max employer contribution, if offered) = $3,150 (combined). This assumes the projected increase to $2,650 for next year is confirmed by the IRS.
Also remember that your health FSA eligibility will need to be no broader than your major medical plan eligibility in order to maintain excepted benefit status. In other words, the health FSA should never be available to an employee who is not also eligible (regardless of enrollment) for your major medical plan.
2018 San Francisco Health Care Security Ordinance (HCSO) Health Care Expenditure Rates
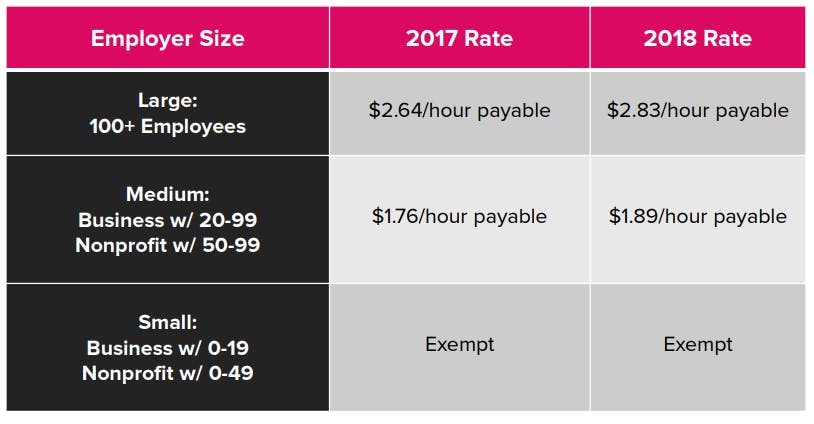
2018 San Francisco Health Care Security Ordinance (HCSO) Expenditure Rates
The San Francisco Office of Labor Standards Enforcement (OLSE) also recently released the updated 2018 HCSO required health expenditure rates.
Under the HCSO, employers with 20 or more employees (50 or more for non-profits) are required to make a minimum level of health care expenditures for certain employees performing work in San Francisco.
The new 2018 rates:
More information on all of these requirements is available on the OLSE’s HCSO website. Also, see our Newfront Office Hours webinar The Health Care Security Ordinance: A Refresher Course in the HCSO Basics for SF Employers (full recording link on the title slide) for a complete overview of the HCSO requirements for employers.
Agencies Issue New ACA Contraception Rule
The ACA requires that non-grandfathered health plans provide coverage for preventive health services without cost-sharing. The preventive care mandate includes preventive services for women, by reference to certain guidelines (without specifically referring to contraception). The Obama administration agencies interpreted this requirement to include coverage for contraception.
The contraceptive mandate has been the subject of extensive litigation, rulemaking, and complex carve-outs since its inception. On Friday, the agencies responsible for ACA enforcements (the Departments of Health and Human Services, Labor, and the Treasury) issued new rules with respect to contraceptive coverage.
The new interim final rules significantly relax the previous requirements for employers with sincerely held religious objections. Most notably, the carve out from the U.S. Supreme Court’s decision in the Hobby Lobby case has been expanded to include for-profit entities that are not closely held, including publicly traded companies.
The rules remain long and complex for employers wishing to invoke the accommodation. Nonetheless, many states include insurances mandates related to contraceptive coverage. Employers that sponsor fully insured plans (and the insurance carriers providing the policies) that are sitused in any of these states will remain subject to those state insurance requirements.
The interim final rules refer to an analysis by the Guttmatcher Institute for state-by-state information for such insurance mandates applicable to fully insured plans. Kaiser Family Foundation has a similar analysis available.
More Fall Reminders
**Medicare Part D: **The Medicare Part D Notice of Creditable (or Non-Creditable) Coverage is due to employees by October 15. Employers frequently bundle this with other required annual notices, such as the CHIP and WHCRA notices.
Form 5500: The Form 5500 filing due date for calendar-year plans that filed that filed for the 2½-month extension is October 16.
ACA Transitional Reinsurance Fee: For the past three years, November has meant another round of the ACA’s Transitional Reinsurance Fee. However, you can scratch item that from your to-do list this year. 2016 was the last year the fee applied.
ACA Reporting: The IRS recently issued the final 2017 Forms 1094-C and 1095-C for employer ACA reporting, as well as updated instructions. The forms remain essentially unchanged from 2016. It is not clear whether the Trump administration will again delay the applicable deadlines or continue the previous years’ good faith enforcement safe harbor.
ACA Premium Tax: The one-year moratorium on the ACA health insurance premium tax will expire at the end of 2017. The 2018 fee will return to the premium for fully insured policies. The tax is estimated to add two to three percentage points to the premium cost.
ACA Pay or Play Penalties: The 2018 employer mandate pay or play penalties increase to $2,320 (the Section 4980H(a) “A Penalty”) and $3,480 (the Section 4980H(b) “B Penalty”) annualized.
ACA Pay or Play Affordability: The 2018 affordability safe harbor percentage decreases from 9.69% to 9.56%. This sets the federal poverty line affordability safe harbor at a $96.08 maximum monthly employee-share of the premium for the lowest-cost plan option at the employee-only tier.

Brian Gilmore
Lead Benefits Counsel, VP, Newfront
Brian Gilmore is the Lead Benefits Counsel at Newfront. He assists clients on a wide variety of employee benefits compliance issues. The primary areas of his practice include ERISA, ACA, COBRA, HIPAA, Section 125 Cafeteria Plans, and 401(k) plans. Brian also presents regularly at trade events and in webinars on current hot topics in employee benefits law.
Connect on LinkedIn